12. Feb, 2022
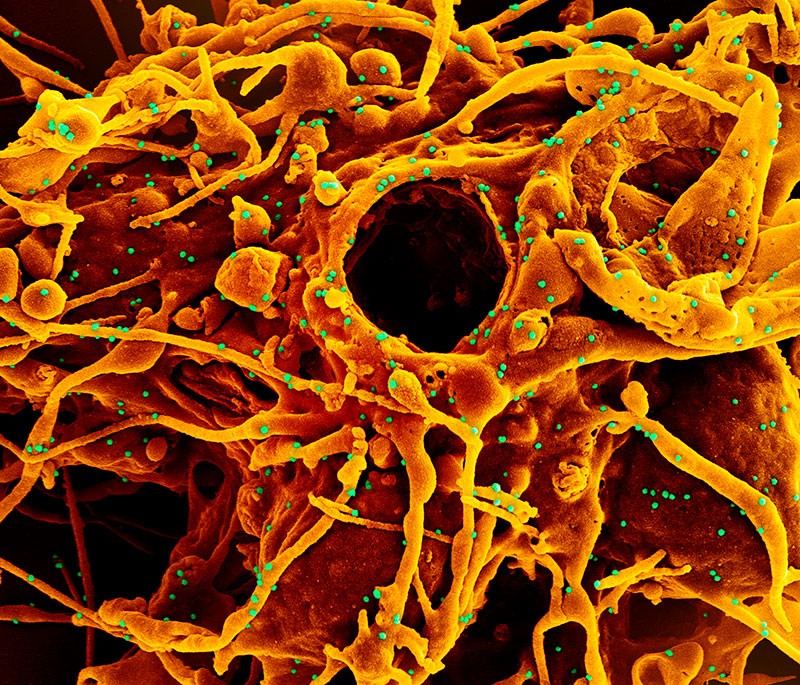
Tvrzení, že SARS-CoV-2 neohrožuje gravidní ženy a nejnovější informace
Opakovaně se objevují informace, že je zbytečné očkovat gravidní ženy, protože je SARS-CoV nijak neohrožuje.
Na toto téma byl v časopise JAMA v lednu 2022 publikován článek:
Association of SARS-CoV-2 Infection With Serious Maternal Morbidity and Mortality From Obstetric Complications
Torri D. Metz, MD, MS; Rebecca G. Clifton, PhD; Brenna L. Hughes, MD, MS; Grecio J. Sandoval, PhD; William A. Grobman, MD, MBA; George R. Saade, MD; Tracy A. Manuck, MD, MS; Monica Longo, MD, PhD; Amber Sowles, BSN, RN; Kelly Clark, BSN, RN; Hyagriv N. Simhan, MD; Dwight J. Rouse, MD; Hector Mendez-Figueroa, MD; Cynthia Gyamfi-Bannerman, MD, MS; Jennifer L. Bailit, MD, MPH; Maged M. Costantine, MD; Harish M. Sehdev, MD; Alan T. N. Tita, MD, PhD; George A. Macones, MD; for the Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units (MFMU) Network
RESULTS Of the 14 104 included patients (mean age, 29.7 years), 2352 patients had SARS-CoV-2 infection and 11 752 did not have a positive SARS-CoV-2 test result. Compared with those without a positive SARS-CoV-2 test result, SARS-CoV-2 infection was significantly associated with the primary outcome (13.4% vs 9.2%; difference, 4.2% [95% CI, 2.8%-5.6%]; adjusted relative risk [aRR], 1.41 [95% CI, 1.23-1.61]). All 5 maternal deaths were in the SARS-CoV-2 group. SARS-CoV-2 infection was not significantly associated with cesarean birth (34.7% vs 32.4%; aRR, 1.05 [95% CI, 0.99-1.11]). Compared with those without a positive SARS-CoV-2 test result, moderate or higher COVID-19 severity (n = 586) was significantly associated with the primary outcome (26.1% vs 9.2%; difference, 16.9% [95% CI, 13.3%-20.4%]; aRR, 2.06 [95% CI, 1.73-2.46]) and the major secondary outcome of cesarean birth (45.4% vs 32.4%; difference, 12.8% [95% CI, 8.7%-16.8%]; aRR, 1.17 [95% CI, 1.07-1.28]), but mild or asymptomatic infection (n = 1766) was not significantly associated with the primary outcome (9.2% vs 9.2%; difference, 0% [95% CI, −1.4% to 1.4%]; aRR, 1.11 [95% CI, 0.94-1.32]) or cesarean birth (31.2% vs 32.4%; difference, −1.4% [95% CI, −3.6% to 0.8%]; aRR, 1.00 [95% CI, 0.93-1.07]). CONCLUSIONS AND RELEVANCE Among pregnant and postpartum individuals at 17 US hospitals, SARS-CoV-2 infection was associated with an increased risk for a composite outcome of maternal mortality or serious morbidity from obstetric complications